This indolent form of B-cell lymphoma is considered a chronic disease and poses unique challenges for affected individuals. Patients may live with follicular lymphoma for many years, often managing anxiety around symptom progression.
The Causes of Follicular Lymphoma
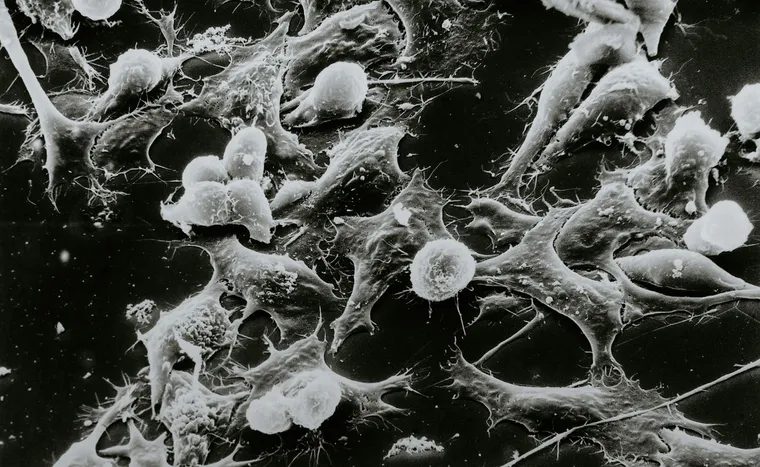
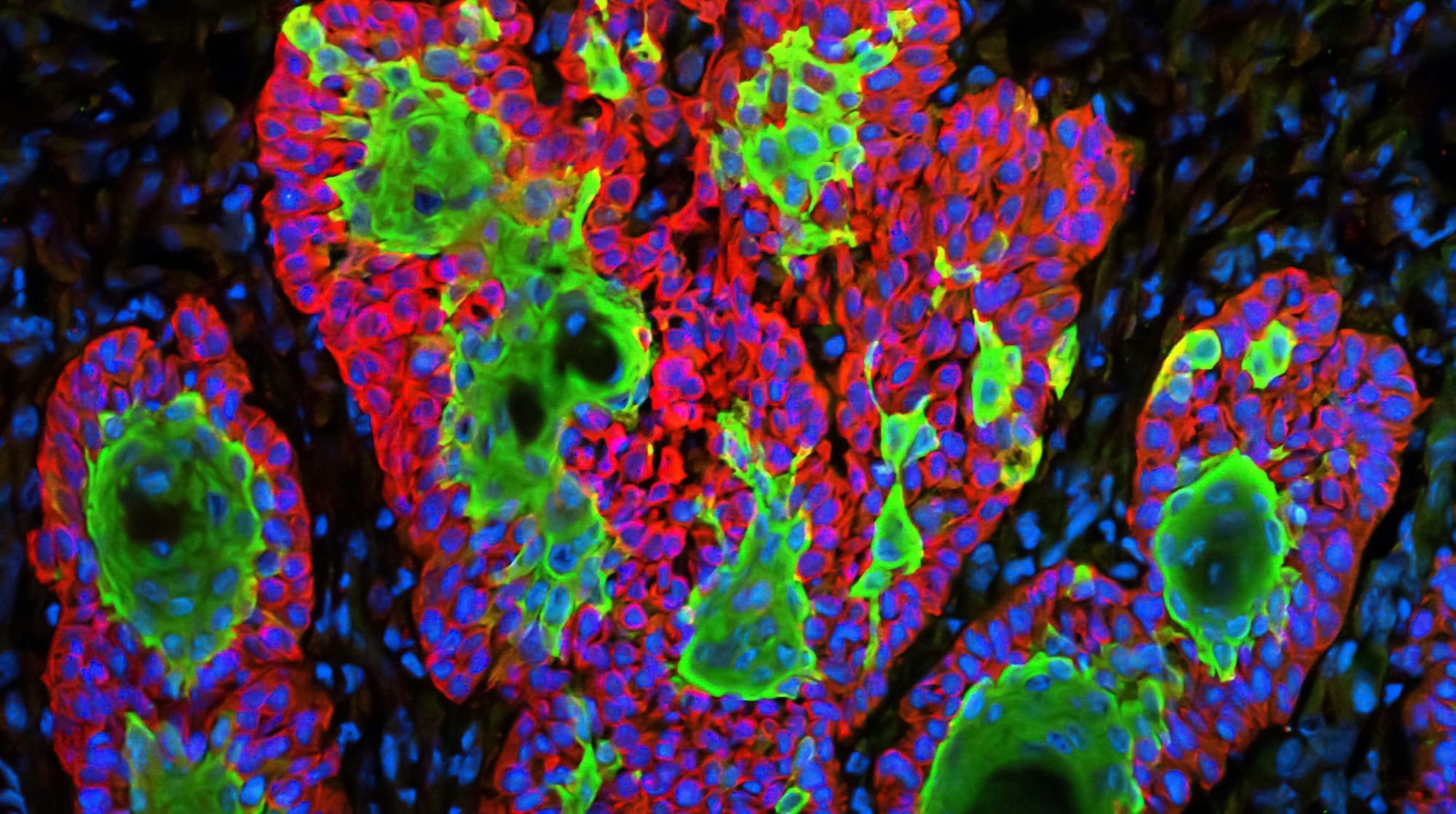
Follicular lymphoma arises from genetic changes in B cells, which lead to the transformation of these cells into malignant entities. These mutations are not inherited but rather develop over time, influenced by various environmental and lifestyle factors. Research points to exposure to toxic chemicals, smoking, and certain infections as potential contributors. Despite these insights, the precise mechanisms that trigger these genetic aberrations remain under scientific scrutiny.
It's worth noting that while the mutations in B cells are a significant factor, the exact cause of follicular lymphoma is multifaceted and not completely understood. This complexity makes it crucial for ongoing research to untangle the interplay between genetic predispositions and environmental influences. Understanding these causes more clearly can pave the way for better preventative measures and targeted treatments, ultimately improving patient outcomes.
Recognizing the Symptoms of Follicular Lymphoma
Follicular lymphoma often presents with symptoms that can easily be mistaken for other illnesses. Initially, you might notice swollen lymph nodes, which can occur in the neck, armpit, or groin. Unlike typical infections, these swollen nodes are usually painless and persist over time. Additionally, you might experience a sense of fullness or discomfort in your abdomen due to an enlarged spleen or liver.
Less common but serious symptoms include fever, night sweats, and unexplained weight loss, often referred to as B symptoms. Some individuals might experience chest pain, frequent coughing, or shortness of breath if the lymph nodes in the chest area are affected. It's essential to pay attention to these signs and consult a healthcare provider for an accurate diagnosis, as early detection can significantly influence the treatment approach and outcome.
Stages of Follicular Lymphoma
Follicular lymphoma is often classified using the Ann Arbor staging system, which helps determine the extent of the disease within the body. This system categorizes the disease into four stages, ranging from stage I to stage IV. In stage I, the cancer is limited to a single lymph node region or a single organ outside the lymph nodes. By the time it reaches stage IV, the lymphoma has spread to one or more organs beyond the lymph nodes, such as the bone marrow, liver, or lungs. Stages II and III represent intermediate levels of spread, involving multiple lymph node regions or adjacent lymph node areas and organs.
The distinction between early and advanced stages is crucial for determining the appropriate treatment strategy. Early-stage follicular lymphoma (stages I and II) might be managed with localized treatments like radiation therapy, while advanced stages (stages III and IV) generally require systemic treatments such as chemotherapy, immunotherapy, or targeted treatments. Understanding the stage of the disease helps both the medical team and patients make informed decisions regarding the best course of action and anticipate the potential outcomes and progression. Though it's slow-growing, follicular lymphoma can behave unpredictably, making staging a vital step in the treatment journey.
Treatment Options for Follicular Lymphoma
Follicular lymphoma, being a type of cancer that often returns, presents unique challenges when it comes to treatment. The treatment strategy typically begins with a "watch and wait" approach, especially for patients who are asymptomatic. This method involves closely monitoring the patient without immediate intervention, allowing them to avoid unnecessary treatments and their associated side effects. However, when treatment becomes necessary, options are diverse and can be customized based on the stage of the lymphoma and the individual's health condition. Lower-stage follicular lymphoma can often be effectively managed with low-dose radiation therapy, which targets the cancer cells while sparing much of the surrounding healthy tissue.
For more advanced stages or when the lymphoma begins to cause symptoms, various systemic therapies come into play. These include immunotherapy, which harnesses the body's immune system to attack the cancer, and chemotherapy, which uses drugs to kill rapidly dividing cancer cells. Single-agent chemotherapy may be sufficient initially, but multiagent chemotherapy might be required for more aggressive cases. Often, a combination of immunotherapy and chemotherapy, known as chemoimmunotherapy, is employed to provide a synergistic effect. Throughout the treatment journey, a coordinated team of medical professionals including oncologists, hematologists, and other specialists work together to tailor the most effective treatment plan, offering patients the best possible outcomes while maintaining quality of life.